Fitness
A brief literature review completed in the spring of 2016, P Callahan.
A short "Hero's Journey" to perhaps make the idea of fitness a more memorable experience.
There is a journey ahead. It will find me. I cannot hide. The journey eventually finds even the most secretive of lairs. To hide is to lose, time or perhaps self. That which is lost cannot be regained.
The journey is that of change. It can be unrelenting or it may even be forgiving. The journey demands fitness. Less is to flirt with failure. There is no honor in failure earned through lack of effort. I deny self and I deny those with whom I travel. They must carry me.
I can choose to be fit, to carry myself. I find fitness waiting for me. Fitness is awareness of mind and body, of self and needs. Fitness is forgiving of my falls, those times when my vision is poor and my footing awash in storms of violence. Fitness, too, lets me celebrate my wins. Fitness is my ally on the journey.
An alliance is one of recognition. I recognize that fitness will make demands of me. Those demands are that I be true to fitness, that I recognize I must keep my body and mind fit to survive the journey. I provide myself with proper nourishment and exercise. I choose my nourishment carefully and deliberately to sustain me. I choose my exercise for endurance. My mind, my essence, is the simple beneficiary. Fitness sustains my essence, the person making a journey of change.
My journey is but limited to my imagination and beliefs. There are limits, though. I must recognize that fitness has limits. Time has limits. The journey will end. In that last moment, I will celebrate with an ally.
How goes your journey? Met your ally?
The definition of fitness has evolved as we have evolved from hunter-gatherers to a highly industrialized society. By the mid-twentieth century the definition of fitness had advanced from individuals who “judged by accomplishments, are fit to carry on their jobs,” to include the supportive qualities of personality to complete the task without undue fatigue or exhaustion.1,2
Fitness, specifically physical fitness, brought focus to guidelines and measurement of proficiency. Fitness expanded beyond the workplace to consider leisure time.3,4 Greater recognition of the measurement and the scope of fitness encouraged educational focus and clarification of definition. Physical activity was defined as any bodily movement produced by skeletal muscles resulting in the expenditure of energy as measured in kilocalories (Cal). This physical activity could be further categorized into, for example, occupational, sports, conditioning, household, or other activities. Exercise was now defined as the physical activity that is planned, structured, and repetitive with the objective of maintaining or improving physical fitness.5,6
The concept of physical fitness emerged as both health and skill-related as characterized by the ability to perform daily activities with vigor with the benefit of lowering the risk of those conditions associated with physical inactivity.7 Health-related physical activity shows more desirable health outcomes across a variety of physical conditions. In general, exercise and physical activity are associated with better quality of life and health outcomes.8 Conversely, physical inactivity is one of the most decisive risk factors for cardiovascular disease (CVD) prevalence and mortality in adults.9
A brief look across lifespan argues for the importance of physical activity. And, one of the best strategies for improving the longterm health is to live healthy from an early life. Exposing children to the enjoyment of physical exercise and creating a pattern of regular physical activity is more desirable than simply promoting childhood physical fitness.10 Active children are generally leaner, have higher peak bone masses, and display healthier cardiovascular profiles. There is also a carryover effect into adulthood with improved health and the likelihood of continuing as a more active adult.11
A twenty-one country analysis of university students showed that regular physical exercise was consistent with a healthy lifestyle and emotional well-being.12 Similarly, in a survey of over 175 000 adults, the proportion of adults reporting fourteen or more unhealthy physical or mental days was lower among those who attained moderate levels of physical activity than physically inactive adults for all age, ethnic, and sex groups.13,14
Even in sedentary older adults, fitness training is found to have benefits for cognition, with the largest benefits occurring for executive-control processes, such as coordination, inhibition, scheduling, planning, and working memory.15,16 There are arguments that regular exercise is associated with a lower risk for dementia.17 Both dietary and exercise modification seem to be strong promoters of healthy aging.18 Physical exercise leads to improved mood, self-concept, self-esteem, and work behavior. It also appears to improve social skills and cognitive functioning.19,20 The evidence suggests that physical activity and exercise probably alleviate some symptoms associated with mild to moderate depression and reduce the symptoms of anxiety and physiological response to stressors.21 Though, excessive physical activity may lead to overtraining and generate psychological symptoms that mimic depression.22
In contrast to depression, emotional well-being is the subjective state of wellness, happiness, and life satisfaction.23 Well-being might be defined as a positive evaluation of one’s life to include positive emotion, engagement, satisfaction, and meaning.24 Quality of life (QOL) is a broad multidimensional concept that usually includes subjective evaluations of both positive and negative aspects of life that extend the definition of quality of health.25 Health-related quality of life (HRQOL) includes aspects of life that affect perceived physical or mental health. Emotional well-being is a primary component of HRQOL and may be independently associated with the incidence of morbidity, or disease, and mortality.26 A growing body of research supports physical exercise as a lifestyle factor that might lead to increased physical and mental health throughout life.27,28 The recommendation by the World Health Organization (WHO) is that adults 18–64 years should do about 150 minutes of moderate-intensity aerobic physical activity throughout the week, or do 75 minutes of vigorous-intensity aerobic physical activity throughout the week.29 Much of the research appears to support the notion of 30 minutes of moderate leisure time physical activity per day on a regular basis may be beneficial on HRQOL. Higher intensity leisure time physical activity is associated with greater HRQOL.30,31
Good nutrition promotes Health-Related Quality of Life (HRQOL) by averting malnutrition, preventing dietary deficiency disease and promoting optimal functioning.32 Though it may seem obvious, it is important to recognize that food security is considered an important risk factor for child health.33 At the opposite end of the age range, older adults are at risk for poor nutrition and frequently experience declining health related quality of life. Nutritional risk along with social support appear to be significant factors associated with HRQOL.34
There appear to be core aspects of a healthy diet that may lower the risk of mortality outcomes for both men and women. These programs include a diet associated with the Healthy Eating Index of 2010 (HEI-2010).35 The Healthy Eating Index (HEI) is a measure of diet quality in terms of conformance with federal dietary guidance. The HEI-2010 captures the key recommendations of the 2010 Dietary Guidelines and, like earlier versions, is used to assess the quality of a given dietary pattern, set of foods, or menu.36 An index, such as HEI-2010, allows measurement relative to the established index criteria and an associated diet forming the basis for meaningful research. Young women whose diets most closely meet the 2010 Dietary Guidelines for Americans, for example, showed lower adiposity.37
Another healthy diet, Harvard’s Healthy Eating Plate, is associated with the Alternative Healthy Eating Index of 2010 (AHEI-2010). Similarly, a Mediterranean diet associated with the Alternate Mediterranean Diet or aMED, and the DASH Eating Plan, associated with the DASH score, lower the risk of mortality. These diets tend to support whole grains, vegetables, fruit, and plant-based proteins.38,39 Other dietary research suggests that high intakes of fruit, vegetables, fish, and whole grains may be associated with a reduced depression risk.40
Currently, in the United States, the U.S. Department of Health and Human Services has forwarded the Healthy People (HP) initiative that provides science-based, 10-year national objectives for improving health. The current HP2020 iteration measures progress toward target attainment of over one thousand health-related objectives and the elimination of health disparities. Specifically, HP2020 seeks to attain longer lives, achieve health equity, create social and physical environments that promote good health, and promote quality of life, healthy development, and healthy behaviors across all life stages.41,42
Process of Fitness
Arguably one of the earliest and more meaningful definitions of fitness might be captured in the statement “run for your life” as having the personal resources to be able to escape danger. Run for your life can also have a different meaning as in promoting physical and other activities to improve the sustainment and quality of life, or the lifelong run for wellness.
Wellness is often defined as a process of learning new life skills and making conscious choices to improve health and quality of life, prolong life, and achieve total well-being. The World Health Organization (WHO) describes these lifestyle changes as occurring across seven dimensions: social, physical, emotional, career, intellectual, environmental, and spiritual.43,44
Exercise
Physical wellness is the process of making choices to create strong bodies with consideration of exercise, nutrition, rest and sleep, responsible sexual choices, and management of stress, injury and illness.45 An essential aspect of physical wellness is that of exercise. A foundational physical fitness plan might begin with consideration of the 2008 Physical Activity Guidelines for Americans. The associated research on the benefits of physical activity is summarized in the following.46
- Regular physical activity reduces the risk of many adverse health outcomes.
- Some physical activity is better than none.
- For most health outcomes, additional benefits occur as the amount of physical activity increases through higher intensity, greater frequency, and/or longer duration
as brisk walking. Additional benefits occur with more physical activity.
- Both aerobic (endurance) and muscle-strengthening (resistance) physical activity are beneficial.
- Health benefits occur for children and adolescents, young and middle-aged adults, and older adults although the exercise process may differ between groups.
- The health benefits of physical activity occur for people with disabilities.
- The benefits of physical activity far outweigh the possibility of adverse outcomes.
The basis of the Physical Activity Guidelines for Americans program is aerobic physical activity whereby adults do 2 hours and 30 minutes a week of moderate-intensity, or 1 hour and 15 minutes (75 minutes) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic physical activity. Aerobic activity is performed in episodes of at least 10 minutes, preferably spread throughout the week. Additional health benefits may be provided by increasing activity to 5 hours a week of moderate-intensity aerobic physical activity, or 2 hours and 30 minutes a week of vigorous-intensity physical activity, or an equivalent combination of both. Muscle-strengthening activities, that involve all major muscle groups, on two or more days per week, is encouraged.
As much as possible, older adults (65 and older) should adhere to the 2 hours and 30 minutes a week of moderate-intensity aerobic physical activity. If chronic conditions exist, then the adult should be as physically active as abilities and conditions allow. Find a level of effort based on understanding of how personal chronic conditions affect ability. Certainly, consider exercises that maintain or improve balance for risk of falling.
Children and adolescents, aged 6 to 17, should exercise 60 or more minutes a day performing moderate- or vigorous-intensity aerobic physical activity, with vigorous-intensity physical activity at least 3 days a week. A part of daily physical activity should include muscle-strengthening on at least 3 days of the week. For example, unstructured exercises, such as playing on playground equipment, climbing trees, and playing tug-of-war. Or structured, such as lifting weights or working with resistance bands. Additionally, part of the daily physical activity should include bone-strengthening on at least 3 days of the week. Common bone-strengthening impact activities include running, jumping rope, basketball, tennis, and hopscotch.47
How does one translate the guidelines into a meaningful exercise program? One method might be to consider your general intentions, preferences and limitations.48
- What are your goals -- Are your interests health, fitness, or performance related?
- What do you enjoy -- Do you prefer team or solitary activities?
- What are your time limits -- How much time can you devote?
- What gear do you need -- What is your budget?
How do we better define these guidelines into something more specific and measurable? We can numerically evaluate just how much activity is occurring across the course of a week. The metabolic equivalent of task (MET), or metabolic equivalent, is a physiological measure describing the energy used for physical activity. More specifically, the MET is the ratio of the rate of energy (calories) expended during an activity to the rate of energy expended at rest. One MET is the energy equivalent expended by an individual while at rest. A 3 MET activity, for example, expends 3 times the energy used by the body at rest. If you were to do an activity of 3 METs intensity for 20 minutes, you would have done 3 × 20 = 60 MET-minutes of physical activity. A range from 500 to 1,000 MET-minutes per week is considered the amount of physical activity necessary to produce health benefits. But, recognize that the higher the minutes the more beneficial the effect.49
Thus, the specific intensity of an aerobic exercise factors into the calculation.
- Light-intensity activities are defined as 1.1 MET to 2.9 METs.
- Moderate-intensity activities are defined as 3.0 to 5.9 METs. For example, walking at 3.0 miles per hour requires 3.3 METs of energy expenditure and is therefore considered a moderate-intensity activity.
- Vigorous-intensity activities are defined as 6.0 METs or more. For example, running at 10 minutes per mile is a 10 MET activity and is therefore classified as vigorous intensity.
There are associated MET values for particular exercises. Some common MET values are 2.5 for gardening, 3.5 for moderate pace walking, 6.0 for swimming, 7.0 for jogging, and 7.5 for general bicycling. You are encouraged to search the extensive Compendium of Physical Activities online to find the MET value for a number of different activities as well as more detailed information on variations of exercises.50
Beyond MET value though, you may be interested in the number of calories you are burning. To convert your body weight from pounds to kilograms divide by 2.2.
(MET value x 3.5 x weight in kg)/200 = calories burned per minute.
For example, consider a 150 lb. (68 kg) person who runs for 30 minutes at a 6 mph pace (10 METs).
(10 mets x 3.5 x 68 kg)/200 = 2380/200 = 11.9 calories burned per minute 11.9 x 30 min = 357 calories burned per 30 minute run.
For health benefits for most adults, the national guidelines suggest burning 1,000 Calories per week. For weight loss and even greater health benefits an expenditure of 2,000 Calories per week is suggested.51
Need some motivation? Some research suggests we can calculate our “fitness age” based on our peak oxygen intake (V02). V02 is correlated to life span. V02 and fitness age can be calculated without a treadmill by using several measurements that include: waist size, resting heart rate, age, sex, and frequency and intensity of exercise.52 An online calculator to determine fitness age can be found at the Norwegian University of Science and Technology, NTNU CERG Fitness Calculator.53
Nutrition
Another aspect of physical wellness is that of nutrition. A foundational dietary plan might begin with a look at several diets that may lower the risk of mortality.54.
HEI-2010 and the 2015-2020 Dietary Guidelines for Americans
A diet adhering to HEI-2010 captures the key recommendations of the 2010 Dietary Guidelines and can be used to assess the quality of a menu. The 2015-2020 Dietary Guidelines for Americans is a revision to the 2010 guidelines and reflects research that demonstrates eating patterns and physical activity can help people achieve and maintain good health and reduce the risk of chronic disease throughout the lifespan. Several
 terms used throughout the 2015-2020 Dietary Guidelines provide an orientation to the guidelines. A dietary pattern or eating pattern describes a customary way of eating or a combination of foods recommended for consumption. Nutrient dense describes foods and beverages that provide vitamins, minerals, and other substances that contribute to adequate nutrient intakes or may have positive health effects, with little or no solid fats and added sugars, refined starches, and sodium. This includes all vegetables, fruits, whole grains, seafood, eggs, beans and peas, unsalted nuts and seeds, fat-free and low-fat dairy products, and lean meats and poultry. Variety describes an assortment of foods and beverages across and within all food groups and subgroups selected to fulfill the recommended amounts without exceeding the limits for calories and other dietary components. The term shift is used to emphasize the need to make substitutions, that is, choose nutrient-dense foods and beverages in place of less healthy choices rather than increasing the overall intake. This focus on shifts in eating patterns is intended to align current dietary intake with recommendations and highlight multiple strategies across all segments of society to promote healthy eating and physical activity behaviors.55, 56 There are five guidelines.
terms used throughout the 2015-2020 Dietary Guidelines provide an orientation to the guidelines. A dietary pattern or eating pattern describes a customary way of eating or a combination of foods recommended for consumption. Nutrient dense describes foods and beverages that provide vitamins, minerals, and other substances that contribute to adequate nutrient intakes or may have positive health effects, with little or no solid fats and added sugars, refined starches, and sodium. This includes all vegetables, fruits, whole grains, seafood, eggs, beans and peas, unsalted nuts and seeds, fat-free and low-fat dairy products, and lean meats and poultry. Variety describes an assortment of foods and beverages across and within all food groups and subgroups selected to fulfill the recommended amounts without exceeding the limits for calories and other dietary components. The term shift is used to emphasize the need to make substitutions, that is, choose nutrient-dense foods and beverages in place of less healthy choices rather than increasing the overall intake. This focus on shifts in eating patterns is intended to align current dietary intake with recommendations and highlight multiple strategies across all segments of society to promote healthy eating and physical activity behaviors.55, 56 There are five guidelines.
- Follow a healthy eating pattern across the lifespan. Choose a healthy eating pattern at an appropriate calorie level to help achieve and maintain a healthy body weight, support nutrient adequacy, and reduce the risk of chronic disease.
- Focus on variety, nutrient density, and amount. Choose a variety of nutrient-dense foods across and within all food groups in recommended amounts.
- Shift to healthier food and beverage choices. Choose nutrient-dense foods and beverages across and within all food groups in place of less healthy choices. Consider cultural and personal preferences to make these shifts easier to accomplish and maintain.
- Support healthy eating patterns for all. Everyone has a role in helping to create and support healthy eating patterns. These social determinants of health and the economics of public health and prevention are similarly echoed in a global manner by the World Health Organization.57
Additionally, the following 2015-2020 Dietary Guidelines recommendations for healthy eating patterns should be applied in their entirety due to the interconnected relationship of each dietary component.
- Consume a healthy eating pattern that accounts for all foods and beverages within an appropriate calorie level.
- A healthy eating pattern includes: a variety of vegetables from all of the subgroups—dark green, red and orange, legumes (beans and peas), starchy, and other; fruits, especially whole fruits; grains, at least half of which are whole grains; fat-free or low-fat dairy, including milk, yogurt, cheese, and/or fortified soy beverages; a variety of protein foods, including seafood, lean meats and poultry, eggs, legumes, and nuts, seeds, and soy products; and oils.
- A healthy eating pattern limits saturated fats and trans fats, added sugars, and sodium.
There are recommended numerical limits in calories to help individuals achieve healthy eating patterns based on their desired weight and lifestyle. These include consuming less than 10 percent of calories per day from added sugars, less than 10 percent of calories per day from saturated fats, less than 2,300 milligrams (mg) per day of sodium, and if alcohol is consumed, it should be consumed in moderation of one drink per day for females and two for males.
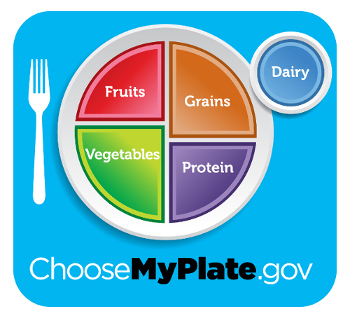
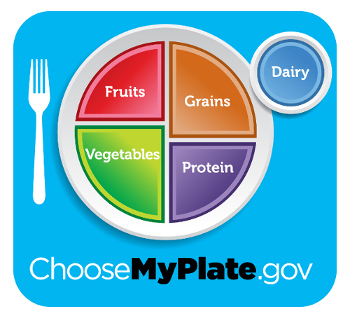
So where does one begin constructing a healthy diet in accord with these guidelines? While the entire guidelines are downloadable, these guidelines can be implemented on such online tools as My Plate (MyPlate) which provides the opportunity to establish personal baseline measures, create a healthy diet, and track fitness related results.58 A basic 2000 Calorie daily menu might look like the following derived from
Supertracker.59
- Breakfast
- 1 ounce(s) Grains
- ½ cup Fruits
- ½ cup( Dairy
- Morning Snack
- 1 ounce(s) Grains
- ½ cup Fruits
- Lunch
- 2 ounce(s) Grains
- 1 cup Vegetables
- ½ cup Fruits
- 2½ ounce(s) Protein Food
- 1 cup Dairy
- Afternoon Snack
- ½ cup Vegetables
- ½ cup Dairy
- Dinner
- 2 ounce(s) Grains
- 1 cup Vegetables
- 3 ounce(s) Protein Food
- 1 cup Dairy
The menu presumes a 2000 Calorie daily plan. Based on variables such as activity, gender, age, height, and
weight, an individual can calculate the appropriate baseline caloric intake for more accurately determining
meal and snack quantities. We want to regulate the total amount of energy, which the body receives through
food intake, and balance this with the total amount of energy that the body expends. Food energy comes into
the body in the form of solids and fluids. The body expends energy through its process of maintaining life,
its digestion and absorption of food, and through physical activity. Overall, we are seeking an energy
balance, where energy balance is the difference between the number of Calories (1000 calories =
1 kilocalories = 1 kcal = 1 Calorie) you eat (intake) and the number of Calories you burn (output). The term
Calorie generally refers to the kilogram calorie. The convention of using the capital C for the kilogram
calorie and the lower case c for the gram calorie is advocated by some, but is not universally
followed.
For men, the following calculation can be used to obtain your Basal Metabolic Rate (BMR) in kcal/day.
66 + (6.23 x weight in pounds) + (12.7 x height in inches) - (6.8 x age in years) or
66 + (13.75 x weight in kg) + (5 x height in cm) - (6.8 x age in years)
For example, a 27-year-old who is 5’11” (71”) tall and weighs 190 lbs.
66 + (6.23 x 190) + (12.7 x 71) – (6.8 x 27) =
66 + 1184 + 902 – 184 = 1,968
For women, the following calculation can be used to approximate the BMR.
655 + (4.35 x weight in pounds) + (4.7 x height in inches) - (4.7 x age in years) or
655 + (9.56 x weight in kilos) + (1.8 x height in cm) - (4.7 x age in years)
For example, a 27-year-old who is 5’ 4” (64”) tall and weighs 120 lbs.
655 + (4.35 x 120) + (4.7 x 64) – (4.7 x 27) =
655 + 522 + 301 – 127 = 1,351
Once the BMR is determined, an activity estimate is identified.
Very Light Seated, standing, driving, computer work 1.2
Light Walking, light stretching, woodworking 1.4
Moderate Jogging, dancing, swimming, biking 1.6
Strenuous Running, soccer, rowing, digging, carrying 1.9
The Harris-Benedict equation can be used to estimate the daily caloric requirement by multiplying the BMR
times the Activity Factor. The obtained value indicates your energy needs or Estimated Energy
Requirement (EER) with the number of Calories of energy you need per day in order to meet your expected
body needs.
EER = BMR x Activity Factor
For example, consider again the 27-year-old male who is 5’11” tall and weighs 190 lbs., his BMR is determined
to be 1968 Cal. and we will assume his Activity Factor is 1.4. Thus, his EER is 1968 x 1.4 or
2755 Cal/day.
Another useful baseline measure is to obtain an approximation of one’s body composition. The Body Mass
Index (BMI) provides an estimate of whether one’s weight is in accord with one’s height. BMI has often
been associated with stress related research. Those with a very low BMI tend to lose weight when
stressed and, conversely, those with a high BMI tend to gain weight when stressed.60,61 Work-related
stress should also be taken into account as having potential impact on weight gain and loss.62
Metabolic Syndrome is the name for a group of risk factors that raises the likelihood for heart disease
and other health problems, such as cancer and diabetes. Characteristics of the metabolic syndrome
include abdominal obesity and high blood pressure.63,64,65,66
BMI = body weight in pounds x 705 / height in inches squared
Alternatively, using an online tool, such as MyPlate Super Tracker, will automatically calculate your
caloric intake and further allow you to set goals such as establishing a preferred body weight and
tracking your results as you progress to your goal. Goal setting shows great promise as a tool that can
be incorporated into weight reduction programs by health care professionals and researchers.67
AHEI-2010 and Harvard’s Healthy Eating Plate
Harvard School of Public Health developed the Alternate Healthy Eating Index (AHEI) with a scoring system
similar to the USDA’s index. AHEI assesses on eleven components to
include dairy products, vegetables, fruit, cholesterol, fat, sodium, alcohol, multivitamins, nuts and seeds,
bread and grains, and fish, poultry and meat.
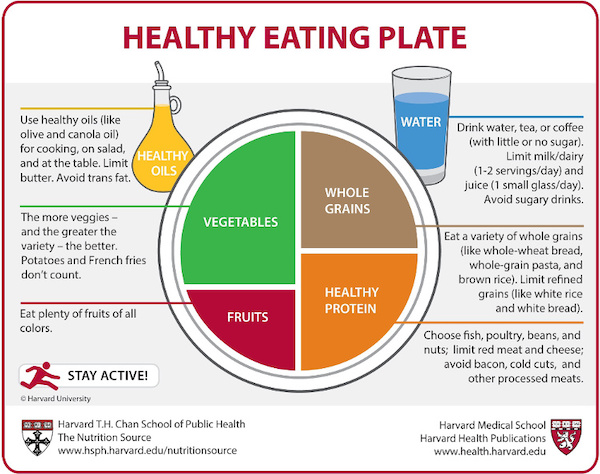
Copyright © 2011, Harvard University. For more information about The Healthy Eating Plate, please see The Nutrition Source, Department of Nutrition, Harvard School of Public Health, www.thenutritionsource.org, and Harvard Health Publications, www.health.harvard.edu.
The Healthy Eating Plate template serves as a concise and functional guide for creating high quality meals.
Based on the plate template, half of your plate is vegetables and fruit. You are encouraged to omit
potatoes, but otherwise aim for color and variety. A quarter of your plate should be whole and intact
grains to include whole wheat, barley, wheat berries, quinoa, oats, brown rice, and foods made with them
such as whole wheat pasta. A quarter of your plate should be protein to include fish, chicken, beans, and
nuts and foods made with them such as salads. Limit red meat, and avoid processed meats such as bacon and
sausage. Healthy plant oils can be used in moderation. Consider olive, canola, soy, corn, sunflower,
peanut, and other oils, but avoid partially hydrogenated oils containing trans fats. Drink water, coffee,
or tea. Omit sugary drinks and limit juice to one small glass per day and milk and dairy products to one
to two servings per day. Finally, you are encouraged to be active for health and weight control.68
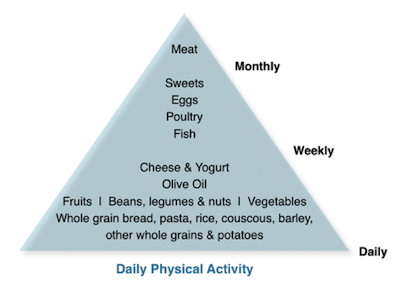
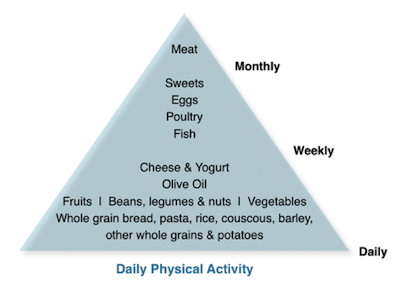
aMED and the Mediterranean Diet
The Mediterranean Diet (MED) and alternate Mediterranean Diet (aMED) are conformity scales for measuring
characteristics of a Mediterranean and modified Mediterranean Diet. There are variations to the diet with
the healthier variants sharing common characteristics as being higher in fresh fruits, root and green
vegetables, whole grains, and fish that is
rich in omega-3 fatty acids, but much lower in red meat. The Mediterranean diets also substitute low or
non-fat dairy products for the high-fat, and further substitute butter and fats for olive oil, nuts or
margarines blended with rapeseed or flaxseed oils.69,70
 A sample one-day sub-2000 Calorie diet might appear much like the following.
A sample one-day sub-2000 Calorie diet might appear much like the following.
- Breakfast
- slice of whole-grain bread
- spread with a tablespoon of nut butter or 2 ounces of avocado
- cup of sliced strawberries with a cup of fruit yogurt
- Lunch
- tossed salad with one-half cup of beans and 1/2 ounce of nuts
- dressing with a tablespoon of olive oil with vinegar or lemon juice and herbs
- Dinner
- baked or grilled, with olive oil, fish, 3 ounces cooked (about 4 ounces raw)
- half-plate serving of vegetables
- ½ cup of whole grain such as brown rice
- Snacks
- cup of plain Greek yogurt with 1/2 cup of blueberries, or
- 1-ounce handful of nuts plus a plate of raw vegetables, or
- 2 Tbsp hummus with 5 whole-grain crackers and a cup of vegetables
There is strong evidence for a beneficial effect of the Mediterranean dietary patterns on risk of death
from all causes, including deaths due to cardiovascular disease and cancer, in a US population.71,72
Similarly, the Mediterranean diet, modified so as to apply across nine European countries, was associated
with increased survival among older people.73
DASH and the DASH Eating Plan
The Dietary Approaches to Stop Hypertension (DASH) diet is a lifelong approach to healthy eating that is
designed primarily to treat or prevent hypertension, but is also consistent with dietary recommendations
to help prevent osteoporosis, cancer, heart disease, stroke and diabetes.74
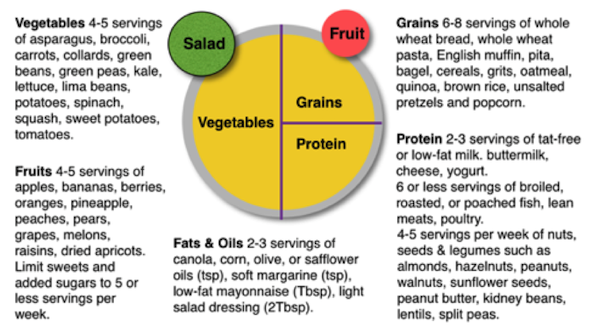 There are two versions of the diet where the standard DASH diet allows up to 2,300 milligrams (mg) of
sodium a day and the lower sodium diet up to 1,500 mg of sodium a day. The diet tends to be low in saturated
fat and cholesterol and therefore encourages vegetables, fruits and low-fat dairy foods with moderate
amounts of whole grains, fish, poultry and nuts.75
There are two versions of the diet where the standard DASH diet allows up to 2,300 milligrams (mg) of
sodium a day and the lower sodium diet up to 1,500 mg of sodium a day. The diet tends to be low in saturated
fat and cholesterol and therefore encourages vegetables, fruits and low-fat dairy foods with moderate
amounts of whole grains, fish, poultry and nuts.75
- Eat vegetables, fruits, and whole grains Including fat-free or low-fat dairy products, fish, poultry,
beans, nuts, and vegetable oils.
- Limit foods that are high in saturated fat, such as fatty meats, full-fat dairy products, and tropical oils
such as coconut, palm kernel, and palm oils.
- Limit sugary beverages and sweets.
Because of the emphasis on lowering blood pressure, the foods are lower in sodium but higher in potassium,
magnesium and calcium. A sample one-day 2000 Calorie diet would assume low salt and might appear much like
the following.76
- Breakfast
- whole-wheat bagel with 2 tablespoons peanut butter (no salt added)
- medium orange
- cup fat-free milk
- Decaffeinated coffee
- Lunch
- Spinach salad made with: 4 cups of fresh spinach leaves, sliced pear, 1/2 cup
canned mandarin orange sections, 1/3 cup slivered almonds, & 2 tablespoons red
wine vinaigrette
- 12 reduced-sodium wheat crackers
- cup fat-free milk
- Dinner
- Herb-crusted baked cod, 3 ounces cooked (about 4 ounces raw)
- 1/2 cup brown rice pilaf with vegetables
- ½ cup fresh green beans, steamed
- small sourdough roll
- 2 teaspoons olive oil
- cup fresh berries with chopped mint
- Herbal iced tea
- Snacks
- cup fat-free, low-calorie yogurt
- 4 vanilla wafers
A more accurate caloric intake can be calculated by factors such as activity level, age, gender, height,
and weight. The number of servings is determined based on the number of calories you are allowed each day.
The caloric intake, can be adjusted upward to gain weight or downward to loose weight. If you intend to
loose weight, it is typically desirable to include exercise as a part of your plan. The following chart,
adapted from the NIH DASH Eating Plan, can be used to determine your servings and serving sizes based on
your nearest caloric grouping.77
DASH Eating Plan Servings Per Day Reference
| | | | |
|---|
| Food Group | 1600 | 2000 | 2600 | Serving Size |
| Grains | 6 | 6-8 | 10-11 | 1 slice bread, 1 oz cereal, ½ cup cooked rice, pasta, or cereal |
| Vegetables | 3-4 | 4-5 | 5-61 | 1 cup raw leafy vegetable, ½ cup raw or cooked vegetable. ½ cup vegetable juice |
| Fruits | 4 | 4-5 | 15-6 | 1 medium fruit, ¼ cup dried fruit, ½ cup fresh, frozen, or canned fruit. ½ cup juice |
| Fat-free or low-fat milk products | 2-3 | 2-3 | 3 | 1 cup milk or yogurt, 1½ oz cheese |
| Lean meats, poultry & fish | 3-6 | 6 or less | 6 | 1 oz cooked meats, poultry, or fish, 1 egg |
| Nuts, seeds & legumes | 3 per week | 4-5 per weekr | 1 | ⅓ cup nuts, 2 Tbsp peanut butter, 2 Tbsp seeds, ½ cup cooked legumes |
| Fats & oils5 | 2 | 2-3 | 3 | 1 tsp soft margarine, 1 tsp vegetable oil, 1 Tbsp mayonnaise, 2 Tbsp salad dressing |
| Sweets & sugars | 0 | 2 or less | 5 or less | 1 Tbsp sugar, 1 Tbsp jelly or jam, ½ cup sorbet, gelatin 1 cup lemonade |
DASH diet with a low sodium level has demonstrated a significant reduction of systolic blood pressure of
around 7 mmHg lower in people without hypertension, and around 11 mmHg lower in people with
hypertension.78,79 Even larger blood pressure reductions occur for overweight or obese persons with the
addition of exercise and weight loss to the DASH diet.80,81
References
1. Penrose, L. S. “The meaning of fitness in human populations.” Annals of eugenics 14, no. 1 (1947): 301-304.
2. Darling, Robert C., Ludwig W. Eichna, Clark W. Heath, and Harold G. Wolff. "Physical fitness: report of the Subcommittee of the Baruch Committee on Physical Medicine." Journal of the American Medical Association 136, no. 11 (1948): 764-767.
3. Fleishman, Edwin A. "The structure and measurement of physical fitness." (1964).
4. Clarke, H. Harrison. "Application of measurement to health and physical education." (1976).
5. Caspersen, Carl J., Kenneth E. Powell, and Gregory M. Christenson. "Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research." Public health reports 100, no. 2 (1985): 126.
6. ACSM’s resource manual for guidelines for exercise testing and prescription. Baltimore, MD: Lippincott Williams & Wilkins, 2006.
7. Pate, Russell R. "The evolving definition of physical fitness." Quest 40, no. 3 (1988): 174-179.
8. Penedo, Frank J., and Jason R. Dahn. "Exercise and well-being: a review of mental and physical health benefits associated with physical activity." Current opinion in psychiatry 18, no. 2 (2005): 189-193.
9. United States. Department of Health. Physical activity and health: a report of the Surgeon General. diane Publishing, 1996.
10. Rowland, Thomas W., and Patty S. Freedson. "Physical activity, fitness, and health in children: a close look." Pediatrics 93, no. 4 (1994): 669-672.
11. Boreham, Colin, and Chris Riddoch. "The physical activity, fitness and health of children." Journal of sports sciences 19, no. 12 (2001): 915-929.
12. Steptoe, Andrew, Jane Wardle, Raymond Fuller, Arne Holte, Joao Justo, Robbert Sanderman, and Lars Wichstrøm. "Leisure-time physical exercise: prevalence, attitudinal correlates, and behavioral correlates among young Europeans from 21 countries." Preventive medicine 26, no. 6 (1997): 845-854.
13. Brown, David W., Lina S. Balluz, Gregory W. Heath, David G. Moriarty, Earl S. Ford, Wayne H. Giles, and Ali H. Mokdad. "Associations between recommended levels of physical activity and health-related quality of life Findings from the 2001 Behavioral Risk Factor Surveillance System (BRFSS) survey." Preventive medicine 37, no. 5 (2003): 520-528.
14. Brown, David W., David R. Brown, Gregory W. Heath, L. I. N. A. Balluz, WAYNE H. Giles, EARL S. Ford, and Ali H. Mokdad. "Associations between physical activity dose and health-related quality of life." Medicine and Science in Sports and Exercise 36, no. 5 (2004): 890-896.
15. Colcombe, Stanley, and Arthur F. Kramer. "Fitness effects on the cognitive function of older adults a meta-analytic study." Psychological science 14, no. 2 (2003): 125-130.
16. Voss, Michelle W., Timothy B. Weng, Agnieszka Z. Burzynska, Chelsea N. Wong, Gillian E. Cooke, Rachel Clark, Jason Fanning et al. "Fitness, but not physical activity, is related to functional integrity of brain networks associated with aging." NeuroImage (2015).
17. Larson, Eric B., Li Wang, James D. Bowen, Wayne C. McCormick, Linda Teri, Paul Crane, and Walter Kukull. "Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older." Annals of internal medicine 144, no. 2 (2006): 73-81.
18. Hammar, Mats, and Carl Johan Östgren. "Healthy aging and age-adjusted nutrition and physical fitness." Best Practice & Research Clinical Obstetrics & Gynaecology 27, no. 5 (2013): 741-752.
19. Folkins, Carlyle H., and Wesley E. Sime. "Physical fitness training and mental health." American Psychologist 36, no. 4 (1981): 373.
20. Plante, Thomas G., and Judith Rodin. "Physical fitness and enhanced psychological health." Current psychology 9, no. 1 (1990): 3-24.
21. Taylor, C. Barr, James F. Sallis, and Richard Needle. "The relation of physical activity and exercise to mental health." Public health reports 100, no. 2 (1985): 195.
22. Paluska, Scott A., and Thomas L. Schwenk. "Physical activity and mental health." Sports medicine 29, no. 3 (2000): 167-180.
23. Diener, Ed. "Subjective well-being: The science of happiness and a proposal for a national index." American psychologist 55, no. 1 (2000): 34.
24. Diener, Ed, and Martin EP Seligman. "Beyond money toward an economy of well-being." Psychological science in the public interest 5, no. 1 (2004): 1-31.
25. Group, The Whoqol. "The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties." Social science & medicine 46, no. 12 (1998): 1569-1585.
26. Galper, Daniel I., Madhukar H. Trivedi, Carolyn E. Barlow, Andrea L. Dunn, and James B. Kampert. "Inverse association between physical inactivity and mental health in men and women." Medicine and Science in Sports and Exercise 38, no. 1 (2006): 173.
27. Hillman, Charles H., Kirk I. Erickson, and Arthur F. Kramer. "Be smart, exercise your heart: exercise effects on brain and cognition." Nature reviews neuroscience 9, no. 1 (2008): 58-65.
28. Bize, Raphaël, Jeffrey A. Johnson, and Ronald C. Plotnikoff. "Physical activity level and health-related quality of life in the general adult population: a systematic review." Preventive medicine 45, no. 6 (2007): 401-415.
29. World Health Organization. "Global recommendations on physical activity for health." (2010).
30. Vuillemin, Anne, Stéphanie Boini, Sandrine Bertrais, Sabrina Tessier, Jean-Michel Oppert, Serge Hercberg, Francis Guillemin, and Serge Briançon. "Leisure time physical activity and health-related quality of life." Preventive medicine 41, no. 2 (2005): 562-569.
31. Tessier, Sabrina, Anne Vuillemin, Sandrine Bertrais, Stéphanie Boini, Etienne Le Bihan, Jean-Michel Oppert, Serge Hercberg, Francis Guillemin, and Serge Briançon. "Association between leisure-time physical activity and health-related quality of life changes over time." Preventive medicine 44, no. 3 (2007): 202-208.
32. Amarantos, Eleni, Andrea Martinez, and Johanna Dwyer. "Nutrition and quality of life in older adults." The Journals of Gerontology series A: Biological sciences and Medical sciences 56, no. suppl 2 (2001): 54-64.
33. Casey, Patrick H., Kitty L. Szeto, James M. Robbins, Janice E. Stuff, Carol Connell, Jeffery M. Gossett, and Pippa M. Simpson. "Child health-related quality of life and household food security." Archives of pediatrics & adolescent medicine 159, no. 1 (2005): 51-56.
34. Keller, H. H. "Nutrition and health-related quality of life in frail older adults." The journal of nutrition, health & aging 8, no. 4 (2003): 245-252.
35. Reedy, Jill, Susan M. Krebs-Smith, Paige E. Miller, Angela D. Liese, Lisa L. Kahle, Yikyung Park, and Amy F. Subar. "Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults." The Journal of nutrition 144, no. 6 (2014): 881-889.
36. Guenther, Patricia M., Kellie O. Casavale, Jill Reedy, Sharon I. Kirkpatrick, Hazel AB Hiza, Kevin J. Kuczynski, Lisa L. Kahle, and Susan M. Krebs-Smith. "Update of the healthy eating index: HEI-2010." Journal of the Academy of Nutrition and Dietetics 113, no. 4 (2013): 569-580.
37. Bailey, Bruce W., Annette Perkins, Larry A. Tucker, James D. LeCheminant, Jared M. Tucker, and Breckann Moncur. "Adherence to the 2010 Dietary Guidelines for Americans and the Relationship to Adiposity in Young Women." Journal of nutrition education and behavior 47, no. 1 (2015): 86-93.
38. Reedy, Jill, Susan M. Krebs-Smith, Paige E. Miller, Angela D. Liese, Lisa L. Kahle, Yikyung Park, and Amy F. Subar. "Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults." The Journal of nutrition 144, no. 6 (2014): 881-889.
39. Chiuve, Stephanie E., Teresa T. Fung, Eric B. Rimm, Frank B. Hu, Marjorie L. McCullough, Molin Wang, Meir J. Stampfer, and Walter C. Willett. "Alternative dietary indices both strongly predict risk of chronic disease." The Journal of nutrition (2012): jn-111.
40. Lai, Jun S., Sarah Hiles, Alessandra Bisquera, Alexis J. Hure, Mark McEvoy, and John Attia. "A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults." The American journal of clinical nutrition (2014): ajcn-069880.
41. Talih M, Huang DT. Measuring progress toward target attainment and the elimination of health disparities in Healthy People 2020. Healthy People Statistical Notes, no 27. Hyattsville, MD: National Center for Health Statistics. 2016.
42. Penman-Aguilar, Ana, Makram Talih, David Huang, Ramal Moonesinghe, Karen Bouye, and Gloria Beckles. "Measurement of health disparities, health inequities, and social determinants of health to support the advancement of health equity." Journal of Public Health Management and Practice 22 (2016): S33-S42.
43 World Health Organization. “The seven dimensions of wellness.” (2007).
44. Hoeger, Wener, and Sharon Hoeger. Lifetime physical fitness and wellness: A personalized program. Cengage Learning, 2016.
45. World Health Organization. “The seven dimensions of wellness.” (2007).
46. “Physical Activity Guidelines for Americans.,” Office of Disease Prevention and Health Promotion, accessed May 30, 2016, http://health.gov/paguidelines/guidelines/summary.aspx
47. Centers for Disease Control and Prevention. Steps to Wellness: A Guide to Implementing the 2008 Physical Activity Guidelines for Americans. Atlanta: U.S. Department of Health and Human Services; 2012.
48. Anita Singh, Tamara L. Bennett and Patricia A. Deuster, Force Health Protection: Nutrition and Exercise Resource Manual (Department of Military and Emergency Medicine Uniformed Services University of the Health Science F. Edward Hebert School of Medicine, 1999), 29.
49. Centers for Disease Control and Prevention. Steps to Wellness: A Guide to Implementing the 2008 Physical Activity Guidelines for Americans. Atlanta: U.S. Department of Health and Human Services; 2012.
50. Ainsworth, B. E., W. L. Haskell, S. D. Herrmann, N. Meckes, D. R. Bassett, C. Tudor-Locke, J. L. Greer, J. Vezina, M. C. Whitt-Glover, and A. S. Leon. "The Compendium of Physical Activities Tracking Guide. Healthy Lifestyles Research Center, College of Nursing & Health Innovation, Arizona State University." Compendium of Physical Activities. accessed May 30, 2016, https://sites.google.com/site/compendiumofphysicalactivities/Activity-Categories
51. Humphrey, Reed. "Clinical Applications: The Exercise Caloric Challenge." ACSM's Health & Fitness Journal 10, no. 2 (2006): 40-41.
52. B. M. Nes, I. Janszky, L. J. Vatten, T. I. Nilsen, S. T. Aspenes and U. Wisløff, “Estimating VO2 peak from a nonexercise prediction model: the HUNT Study, Norway,” Med Sci Sports Exerc 43 no. 11 (2011): 2024-30, accessed January 13, 2014, doi: 10.1249/MSS.0b013e31821d3f6f.
53. “Fitness Calculator,” Norwegian University of Science and Technology, accessed May 30, 2016, https://www.ntnu.edu/cerg/vo2max
54. Reedy, Jill, Susan M. Krebs-Smith, Paige E. Miller, Angela D. Liese, Lisa L. Kahle, Yikyung Park, and Amy F. Subar. "Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults." The Journal of nutrition 144, no. 6 (2014): 881-889.
55. U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. 8th Edition. December 2015. Available at http://health.gov/dietaryguidelines/2015/guidelines/.
56. DeSalvo, Karen B., Richard Olson, and Kellie O. Casavale. "Dietary Guidelines for Americans." JAMA (2016): 1-2.
57. World Health Organization (WHO. "Health 2020. A European policy framework and strategy for the 21st century." MPs (2015).
58. U.S. Department of Agriculture. ChooseMyPlate.gov Website. Washington, My Plate. www.choosemyplate.gov. Accessed May 5, 2016.
59. “Sample Meal Plans,” Supertracker, accessed May 30, 2016, https://supertracker.usda.gov/samplemealplans.aspx
60. EPEL, ELISSA, SHERLYN JIMENEZ, KELLY BROWNELL, LAURA STROUD, CATHERINE STONEY, and RAY NIAURA. "Are stress eaters at risk for the metabolic syndrome?." Annals of the New York Academy of Sciences 1032, no. 1 (2004): 208-210.
61. Susan Torres and Caryl Nowson, “Relationship Between Stress, Eating Behavior and Obesity,” Nutrition 23 no. 11-12, (2007): 887-894.
62. Kivimäki, M., J. Head, J. E. Ferrie, M. J. Shipley, E. Brunner, J. Vahtera, and M. G. Marmot. "Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study." International journal of obesity 30, no. 6 (2006): 982-987.
63. Räikkönen, Katri, Karen A. Matthews, and Lewis H. Kuller. "Depressive symptoms and stressful life events predict metabolic syndrome among middle-aged women a comparison of World Health Organization, Adult Treatment Panel III, and International Diabetes Foundation definitions." Diabetes care 30, no. 4 (2007): 872-877.
64. Ford, Earl S., Wayne H. Giles, and Ali H. Mokdad. "Increasing prevalence of the metabolic syndrome among US adults." Diabetes care 27, no. 10 (2004): 2444-2449.
65. Marchesini, Giulio, Elisabetta Bugianesi, Gabriele Forlani, Fernanda Cerrelli, Marco Lenzi, Rita Manini, Stefania Natale et al. "Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome." Hepatology 37, no. 4 (2003): 917-923.
66. Esposito, Katherine, Paolo Chiodini, Annamaria Colao, Andrea Lenzi, and Dario Giugliano. "Metabolic Syndrome and Risk of Cancer A systematic review and meta-analysis." Diabetes Care 35, no. 11 (2012): 2402-2411.
67. Pearson, Erin S. "Goal setting as a health behavior change strategy in overweight and obese adults: a systematic literature review examining intervention components." Patient education and counseling 87, no. 1 (2012): 32-42.
68. Willett, Walter C. "Eat, drink, and be healthy." (2001).
69. Goff, David C., Donald M. Lloyd-Jones, Glen Bennett, Sean Coady, Ralph B. D’Agostino, Raymond Gibbons, Philip Greenland et al. "2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines." Journal of the American College of Cardiology 63, no. 25_PA (2014).
70. Preedy, Victor R., Lan-Anh Hunter, and Vinood B. Patel, eds. Diet quality: an evidence-based approach. Vol. 2. Springer Science & Business Media, 2013, p56.
71. Mitrou, Panagiota N., Victor Kipnis, Anne CM Thiébaut, Jill Reedy, Amy F. Subar, Elisabet Wirfält, Andrew Flood et al. "Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study." Archives of Internal Medicine 167, no. 22 (2007): 2461-2468.
72. Fung, Teresa T., Kathryn M. Rexrode, Christos S. Mantzoros, JoAnn E. Manson, Walter C. Willett, and Frank B. Hu. "Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women." Circulation 119, no. 8 (2009): 1093-1100.
73. Trichopoulou, Antonia, Philippos Orfanos, Teresa Norat, Bas Bueno-de-Mesquita, Marga C. Ocké, Petra HM Peeters, Yvonne T. van der Schouw et al. "Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study." Bmj 330, no. 7498 (2005): 991.
74. Fung, Teresa T., Stephanie E. Chiuve, Marjorie L. McCullough, Kathryn M. Rexrode, Giancarlo Logroscino, and Frank B. Hu. "Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women." Archives of internal medicine 168, no. 7 (2008): 713-720.
75. “Description of the DASH Eating Plan ,” National Institute of Health, accessed May 30, 2016, http://www.nhlbi.nih.gov/health/health-topics/topics/dash/
76. “Sample menus for the DASH diet,” Mayo Clinic, accessed May 30, 2016, http://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/dash-diet/art-20047110
77. “Following the DASH Eating Plan,” NIH Publication No. 06-5834, accessed May 30, 2016, https://www.nhlbi.nih.gov/files/docs/public/heart/dash_brief.pdf
78. Sacks, Frank M., Laura P. Svetkey, William M. Vollmer, Lawrence J. Appel, George A. Bray, David Harsha, Eva Obarzanek et al. "Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet." New England journal of medicine 344, no. 1 (2001): 3-10.
79. Vollmer, William M., Frank M. Sacks, Jamy Ard, Lawrence J. Appel, George A. Bray, Denise G. Simons-Morton, Paul R. Conlin et al. "Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial." Annals of internal medicine 135, no. 12 (2001): 1019-1028.
80. Blumenthal, James A., Michael A. Babyak, Alan Hinderliter, Lana L. Watkins, Linda Craighead, Pao-Hwa Lin, Carla Caccia, Julie Johnson, Robert Waugh, and Andrew Sherwood. "Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study." Archives of internal medicine 170, no. 2 (2010): 126-135.
81. Appel, Lawrence J., Catherine M. Champagne, David W. Harsha, Lawton S. Cooper, Eva Obarzanek, Patricia J. Elmer, Victor J. Stevens et al. "Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial." JAMA: Journal of the American Medical Association (2003).
82. Hudd, Suzanne S., Jennifer Dumlao, Diane Erdmann-Sager, Daniel Murray, Emily Phan, Nicholas Soukas, and Nori Yokozuka. "Stress at college: Effects on health habits, health status and self-esteem." College Student Journal 34, no. 2 (2000): 217-228.
83. Kristjánsson, Álfgeir Logi, Inga Dóra Sigfúsdóttir, and John P. Allegrante. "Health behavior and academic achievement among adolescents: the relative contribution of dietary habits, physical activity, body mass index, and self-esteem." Health Education & Behavior 37, no. 1 (2010): 51-64.
 terms used throughout the 2015-2020 Dietary Guidelines provide an orientation to the guidelines. A dietary pattern or eating pattern describes a customary way of eating or a combination of foods recommended for consumption. Nutrient dense describes foods and beverages that provide vitamins, minerals, and other substances that contribute to adequate nutrient intakes or may have positive health effects, with little or no solid fats and added sugars, refined starches, and sodium. This includes all vegetables, fruits, whole grains, seafood, eggs, beans and peas, unsalted nuts and seeds, fat-free and low-fat dairy products, and lean meats and poultry. Variety describes an assortment of foods and beverages across and within all food groups and subgroups selected to fulfill the recommended amounts without exceeding the limits for calories and other dietary components. The term shift is used to emphasize the need to make substitutions, that is, choose nutrient-dense foods and beverages in place of less healthy choices rather than increasing the overall intake. This focus on shifts in eating patterns is intended to align current dietary intake with recommendations and highlight multiple strategies across all segments of society to promote healthy eating and physical activity behaviors.55, 56 There are five guidelines.
terms used throughout the 2015-2020 Dietary Guidelines provide an orientation to the guidelines. A dietary pattern or eating pattern describes a customary way of eating or a combination of foods recommended for consumption. Nutrient dense describes foods and beverages that provide vitamins, minerals, and other substances that contribute to adequate nutrient intakes or may have positive health effects, with little or no solid fats and added sugars, refined starches, and sodium. This includes all vegetables, fruits, whole grains, seafood, eggs, beans and peas, unsalted nuts and seeds, fat-free and low-fat dairy products, and lean meats and poultry. Variety describes an assortment of foods and beverages across and within all food groups and subgroups selected to fulfill the recommended amounts without exceeding the limits for calories and other dietary components. The term shift is used to emphasize the need to make substitutions, that is, choose nutrient-dense foods and beverages in place of less healthy choices rather than increasing the overall intake. This focus on shifts in eating patterns is intended to align current dietary intake with recommendations and highlight multiple strategies across all segments of society to promote healthy eating and physical activity behaviors.55, 56 There are five guidelines.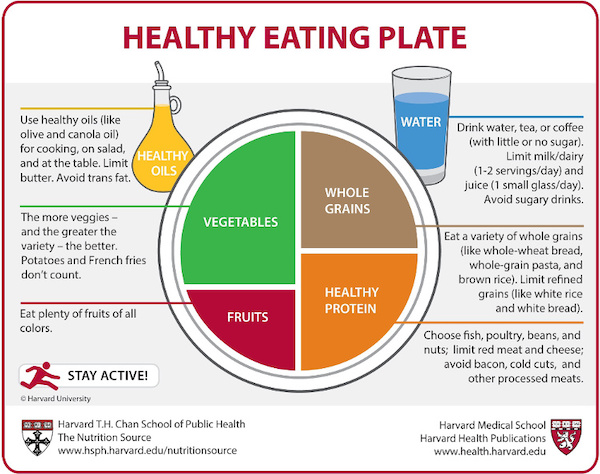
 A sample one-day sub-2000 Calorie diet might appear much like the following.
A sample one-day sub-2000 Calorie diet might appear much like the following.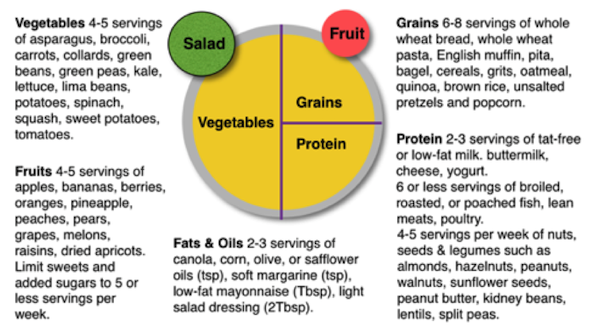 There are two versions of the diet where the standard DASH diet allows up to 2,300 milligrams (mg) of
sodium a day and the lower sodium diet up to 1,500 mg of sodium a day. The diet tends to be low in saturated
fat and cholesterol and therefore encourages vegetables, fruits and low-fat dairy foods with moderate
amounts of whole grains, fish, poultry and nuts.75
There are two versions of the diet where the standard DASH diet allows up to 2,300 milligrams (mg) of
sodium a day and the lower sodium diet up to 1,500 mg of sodium a day. The diet tends to be low in saturated
fat and cholesterol and therefore encourages vegetables, fruits and low-fat dairy foods with moderate
amounts of whole grains, fish, poultry and nuts.75